Hello this is where the tips, questions and answers from the Q and A on Oct 23 2020 will be posted. The 2020 Q and A will run on Oct 23 at 9am to 5pm. (mountain time in Calgary). PLEASE DO NOT hit the refresh button multiple times as a hundred users refreshing the same page will CRASH THE SERVER for the entire night!!! It will take me 15-30 minutes to answer questions so please only hit refresh every 60 minutes. You can email me your 2-3 questions at cdestudycourse@gmail.com. Note I may not get to every question. It is first come first serve. My responses are in BOLD
The password to the Zoom meetings is CDE2020
For the 1-2 pm (mountain time) session the link is: https://us02web.zoom.us/j/8115
For the 4-5:30 pm (mountain time) session the link is: https://us02web.zoom.us/j/8259
Tips
1) Remain calm and go with the answer that you first selected. The people I know that have failed the test panicked and kept changing their answers. Everyone is nervous and that is normal, especially if this is the first time you are writing. Even I was nervous, even though I have taught dozens of other people, have written the exam before and have created tests. Take a few deep breathes and remain calm.
2) Do not waste too much time on any one question. You have 165 questions in 3.5 hours so 1.25 minutes per question. Remember there are twenty five “pilot” questions that are simply being tested and do not count. So if you spend 10 minutes on a tricky question that is worth nothing then you have wasted a lot of time.
3) Read the question slowly and carefully.
Some questions will ask “which of the following is correct” and some questions will ask “which of the following is incorrect“. I caught myself choosing the wrong answer because I did not read the question carefully at first.
Some questions will give you answers that are like a long list. For example
Which of the following are all fruits?
A) Cakes, watermelons, apples, oranges and blueberries
B) Cantaloupes, watermelons, mangoes, pears and doughnuts
C) Apples, oranges, bananas, cherries and raspberries
The key to answering these questions is to look for the ones that are wrong first. Once you see cakes and doughnuts you know the answer is C. This helps you narrow down the possible answers.
Hi Esmond,
Please see the attached Travel Guidelines handout from Alberta Diabetes Link (www.albertadiabeteslink.ca) C-endo’s Diabetes Education website with information for patients and professionals.
Please feel free to let your participants know about the website and that they can use any of the handouts in their own practice!
Steph Tilley BSc, RD, CDE
C-Endo Clinic (Dr Sue Pedersen’s clinic)
Hi Esmond. I am still confused about premix insulin composition ,peak and duration of action. Also I was wondering if there is benefit to using dpp 4 inhibitors with glp1 agonists given the cost.
I have 2 main questions:
1- During live session with Dr Pederson, a question regarding Insulin dose adjustment in time zone change came up and she mentioned that she’ll send some case study. I’m not sure if I cannot find it or it’s not there. I need some more explanation regarding dose adjustment.
2- Difference between Dawn phenomenon and Symogi effect and how to diagnose and differentiate and treatment for Dawn phenomenon.Regards,
Sepi
Hello Esmond,
Your website is so helpful. Thank you so much for taking the time to create all the VERY helpful materials!
Hi Esmond I have difficulty understanding how to calculate the insulin sensitivity factor. Thank you for the tip for 100 divided by total daily dose.
60 Q quizz: Question 20 of 60
You mention that the formula for calculating insulin sensitivity factor (ISF) or Corrector factor (CF) is 100/Total daily dose if using rapid insulin, and 83/TDD if using short acting insulin.
If patient is on 60+60+40+20+20=200. Therefore, 100/200 =0.5.
Meaning 1 unit of insulin is expected to bring him down 0.5 mmol/L? I do not understand this. May you please explain what it means..?
Hi Madonna
That is correct this patient needs 1 unit to bring him down 0.5 mmol/L. If his target was 7 and he was at 9 he would need 4 units. If another person has a ISF of 1:2 then that patient would only need 1 units to bring him down from 9 to 7.
I also do not understand well question 50: most resistant to insulin?
Thank you so much!
Madonna
For this question you need to calculate who has the most resistant ratio as that person is the most resistant to insulin. In the example in the previous question the person with the ISF of 1:0.5 mmol/l or 1:2 mmol/L. Who is most sensitive? The patient with the ISF of 2 mmol b/c he needs less insulin to bring him down.
Try thinking of this way. You punch a sumo wrestler with 1 unit of force and he moves 0.5 meters. You then punch an anorexic girl with 1 unit of force and she moves 2 meters and falls down. Who is more sensitive to your punch? The anorexic girl
Now switch the scenario for diabetes. You inject a sumo wrestler with 1 unit of insulin and his sugars drop 0.5 mmol/L. You inject a anorexic girl with 1 unit of insulin and her sugars drop 2.0 mmol/L and she has a low and faints. Who is more sensitive?
Hi Esmond,
Hi esmond ,
I am reviewing the questions on Essentials. The question 29, regarding benefits of exercise confused me. Does exercise improve glycemic control for type1? The feedback answer is D, all of the above. But I remember exercise doesn’t help glycemic control in type i patients. Please clarify. Thanks!
Xiao
Hi Esmond,
Hi Esmond ,
Hi Esmond,
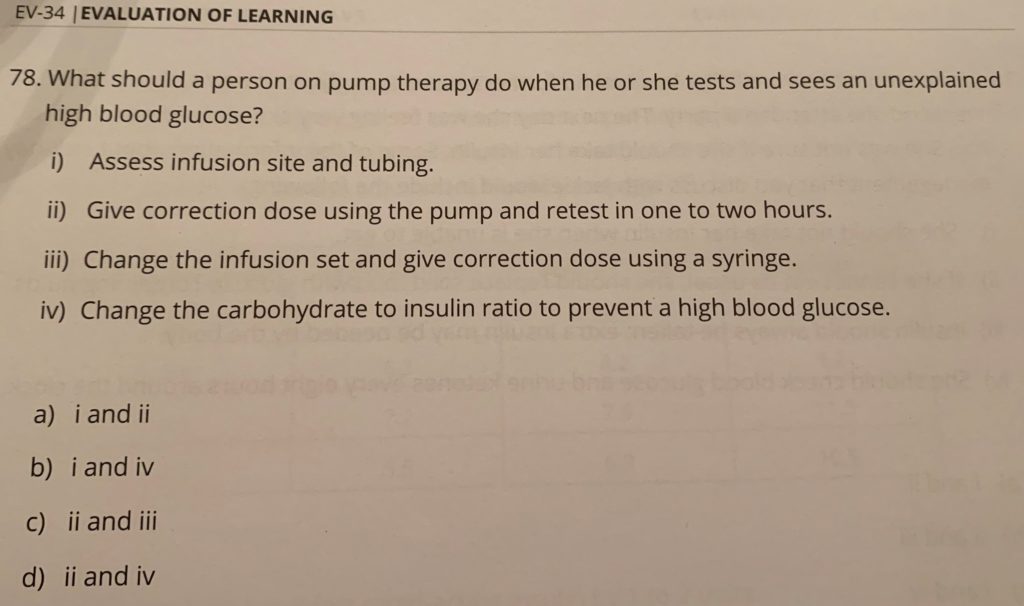
I would think that the answer could be any of the first three? Not sure how I can only pick two…
Shairoz
Hi Sharioz the answer is A. Unexpected lows could be due to infusion site malfunction but it could also be extra sugar the patient did not account for, pt is ill, pt took corticosteroids etc. There are lots of reasons for unexpected lows even though the first thing to suspect is infusion site malfunction. iii is wrong because if the infusion site is properly working you just used a syringe for no reason. iv is wrong because you wouldnt change the ratio based on one reading it should be a patter of highs after using the ratio.
Could you please help with this question ? Bisi
Hello Bisi, I was able to use Paint to improve the resolution of the picture. Its still blurry but I think the answer is C. How you solve the answer is add all the insulin together to find the TDD (total daily dose) which is 35. Then take 60% as bolus and 40% as basal. 60% of 35 is 21 then divide by 3 meals is 7 units with each meal. 40% of 35 is 17. So that is answer C. Thanks
Hello Esmond
I see you are getting a lot of questions already. I am sorry to add to your work load!
Can you please help me understand all the different ways of calculating out insulin and it what scenario to use it:
Essential 5th Edition offers several methods:
- Pg 6-93 for premixed insulin therapy “initiate at 5-10 units once or twice daily or a dose of 0.5 Units/kg/day” does this imply a client can be started on 20 U NPH? No, pre-mixed insulin is not the same as NPH so there is no implication
- Pg 6-88 Basal “initiate at dose of 10 units once daily or 0.1 to 0.2 Units/kg” this is the same as the guidelines. However I would imagine if the client is obese the best option would be to calculate. Yes, if you have a client that’s very obese he may need 100+ units of insulin to be well controlled. Starting at 10 and increasing by 1 would take months to get to target and would be discouraging for the patient
the dose based on the weight rather than starting at 10 units. Perhaps the same idea for an underweight person.
- Pg 6-91 “calculate the total daily dose: 0.3 to 0.5 Units/Kg or the sum of the individual’s current insulin doses. When would the first part of this sentence be used? The first part would be for a person not on insulin. The second part would be for a person who is one some other regimen like mixed insulin
- Pg 6-69 Type 2 Diabetes: the average total daily dose TDD requirement is 1.0 to 1.5 units/kg/day however can be up to 2.0 units/kg/day. What is insulin dosing method would you use for a T1DM client? Neither I find those averages to be too general and adjust the dosage based on the patients response. I completely ignore the average dose requirements.
- I have been told NPH is a good choice for managing elevated blood glucose from prednisone use. Have you found this effective in your experience? I have found NPH effective for treating hyperglycemia with prednisone. NPH follows the prednisone induced peak in sugars nicely
- Pg 6-87 have you come across any studies that state smoking reduces the rate of rapid and short acting insulin absorption? I have not
- When switching a client from Insulin Aspart to FIASP would you caution the client to lower the dose? No FIASP just works 5 min faster so there is no need to decrease the dose.
Thanks again,
Mary
Hi Esmond,
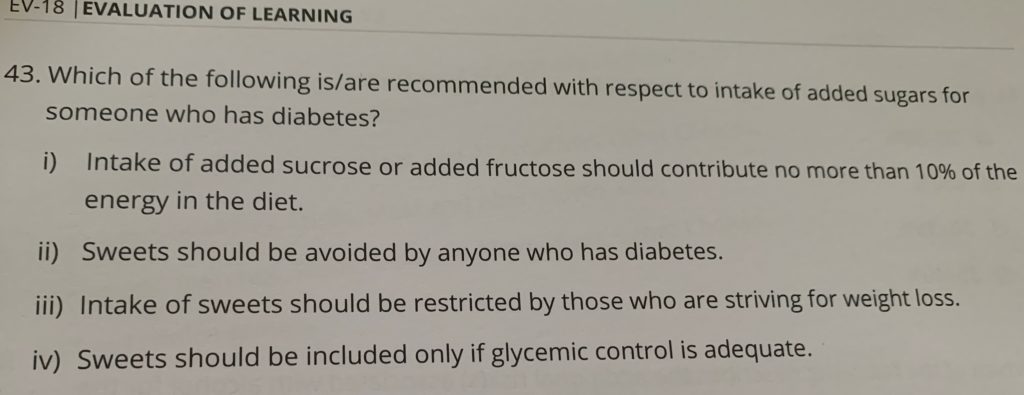
According to essentials answer sheet their answer is BThank you :)Shairoz
Hi Shairoz
The official answer to this question is B but I would have gone with A. i is correct and ii is wrong. However I would say iv is wrong as well. If the patient’s sugars are high I would still want them to enjoy sweets on special occasions as we work towards their target. I think iii is correct so would have gone with A.
Thanks
Esmond
Esmond
Hello Esmond,
I hope this is not too late. Here are some questions for you:
– Similar to a question asked already, but to diagnose DM, you need 2 values in the diabetes range (if asymptomatic to hyperglycemia). So, if only one value is in the range, let’s say the A1C, it would be preferable to retest the A1C right? Preferably you want a different test. And vice versa, if FPG is in the diabetes range, but A1C is normal, you retest the FPG? (Except for random plasma glucose, which is recommended to use an another kind of test)? Look at figure 1 on p S18. There is a fine print that says if discordant use the right most side of the algorithm. I would probably retest using a different test.
– Could you explain the mechanism behind some factors affecting A1C such as erythrocyte pH, vitamin C/E, aspirin, alcoholism…? Some of the mechanisms affect the rate of glycosylation of the hemoglobin. Think of it as different coatings to prevent rust or accelerate rust. This doesn’t affect the actual blood sugar but affects how fast the glycosylation is occurring which is what an A1c test measures.
– When on a certain regimen of MDI and you want to switch to another regimen MDI, there is no dose reduction? When looking on your insulin calculation cheat sheet and the question you answered above, there was no reduction? There are no special adjustments for this.
I assume if you go from twice daily to once daily long acting OR from Toujeo to Lantus, for example, you would need to consider the dose reduction then right? For twice daily to once daily yes for sure. For Toujeo or Lantus not necessarily though it would be an ok idea just to be cautious. Thanks Esmond
I also have been reading the Q&A. I saw a question asked regarding the renal load and low carbohydrate diet. As a dietitian, this would be explained by higher protein intake if carbohydrate intake is reduced. Meaning, kidneys have more protein to filter.
Thank you so much for your time and devotion to help us. :)
Josée
Hi Esmond,
Hi Esmond,
I see that sometimes % is used when adjusting insulin (e.g. reduce basal by 10%). I always went with the 1-2 units per day rule. When do we use % and how would we determine how much percentage?
Thanks,
Lorraine
Hello Lorraine, it depends on the patient. If the patient is a moderate dose of insulin or higher around 30+ units of insulin then I start increasing by 10%. I have one patient who is on 300 units of Toujeo so going up by 1 unit daily would take a forever to get to target.
Hi Esmond, I forgot to ask about travel questions. how detailed are the question son insulin and travel and can you give some tips to easily remember timezones an insulin changes. I will join again at 4 pm
Hi Marleis, you don’t have to memorize the timezones for the exam. Just know if you are losing time you need to decrease the insulin and if you are increasing time then you dont increase the basal you would just do another extra bolus. In real life you could just switch to Tresiba and not have to deal with these time zone differences. Hopefully they will have that as an option on the exam!
Hi Esmond, me again. one more question regarding autonomic complications. Can you speak this. Why is reduced sensation in the feet not an autonomic complication?
Hi Marleis, I can see your referring to Question #17 of the Essentials. Im not sure why the answer is C. I guess that all the other options such as anyhyrosis, orthostatic hypotension, and gastropareis dont involve thiking or sensing?
Hey Lorraine just answered this question. Its because loss of sensation is considred to be a sensorimotor neuropathy not autonomic. Thanks Esmond